Perhaps Leona Ellis enjoyed too much good fortune. A salon owner who worked four days a week, Ellis spent her free time in northern Michigan kayaking, bicycling, rollerblading, cross-country skiing, and snowshoeing. But two years ago, seemingly out of the blue, Ellis began suffering from overwhelming fatigue, even following nights when she slept well.
As time passed, her problems multiplied. Her body began to ache; first in her knees, then traveling to her hips, her quadriceps, and buttocks. The pain was compounded by severe muscle spasms in her legs. “By August and September of 2007,” she recalls, “it was almost impossible to bend over and pick something up. [My] muscles didn’t feel like they would stretch that far. I was in constant pain.” Visits to her regular internist were met with quizzical looks and assurances that her blood levels were normal. She was told to take ibuprofen and an antidepressant. “I lived out of that ibuprofen bottle to keep going,” she says.
By November, the muscle spasms and aches had progressed to Ellis’ shoulders, and she was bedridden. A visit to an urgent-care clinic suggested a virus. Following Christmas — some 18 months after the first symptoms appeared — her internist suggested she might be suffering from fibromyalgia.
First diagnosed in 1990 by the American College of Rheumatology, fibromyalgia is recognized by most doctors as a disabling illness, although some still see it as a more psychological malady. Because fibromyalgia is a relatively new disease, proper diagnosis and successful treatment can take months, or even years, with patients running the gamut of medical specialists.
Lisa Meloche, a 36-year-old therapist from Sterling Heights, believes she may have been suffering from some form of fibromyalgia most of her life. “I was tested for mono many times, my legs ached, and I couldn’t get answers why,” she says. Meloche was finally diagnosed in 1999, after having physical therapy for sciatica. There were also terrible headaches, thyroid problems, severe menstrual cycles, carpal tunnel syndrome, irritable-bowel syndrome, insomnia, and aches and pains all throughout her body. She was extremely sensitive to varying temperatures, as well.
Yet she was reluctant when she heard the diagnosis, concerned that it wasn’t a “real” disease.
But new research has helped people recognize fibromyalgia as a disease. “The development of two new drugs, Cymbalta and Lyrica, has validated [for] many doctors that it is a real disorder, not just a trashcan disorder,” says Dr. Gamal Wazni, principal of Fibromyalgia & Fatigue Centers Inc. in Troy. According to the National Institutes of Health, however, Lyrica (Pfizer’s trade name for pregabalin) has caused decreased fertility in male animals, as well as birth defects in the offspring of male and female animals who were treated with the medication.
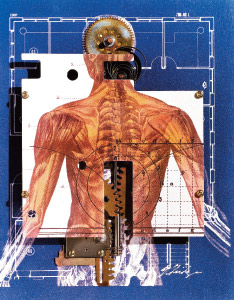
Some researchers believe that a central-nervous-system malfunction is what causes fibromyalgia. Others believe that fibromyalgia is caused by a lack of deep REM (stage 4) sleep, when the muscles recover from the previous day’s activities. Other researchers feel that it’s triggered by a virus, which causes the body’s nerves to misfire. Symptoms can vary from person to person, but there are several that are commonly shared by most sufferers — 90 percent of whom are women.
Approximately 6 million people, or 2 percent of the population, have fibromyalgia. Typically, fibromyalgia patients experience severe aches and pain in the muscles, tendons, and joints, especially along the spine. In turn, specific areas of the body — often called trigger points — can be extremely tender to the touch.
Additionally, sleep disturbances, notably insomnia, are often associated with the pain, as well as headaches, fatigue, chest pain, morning stiffness, anxiety, depression, irritable bowel syndrome, and cognitive memory impairment known as a “fibro fog.” Hormonal imbalances, which cause women to experience painful menstrual cramps, skin problems, and infertility, are also common. Patients can also suffer from other overlapping health conditions, such as chronic-fatigue syndrome, temporomandibular joint syndrome, restless-leg syndrome, myofascial pain syndrome, and multiple-chemical sensitivity. In other words, they’re a mess.
Ellis’ doctor discovered she had a virus called Epstein-Barr, which causes mononucleosis and chronic-fatigue syndrome, in addition to fibromyalgia. After some diligent research, she came across Dr. Wazni. “What we know about fibromyalgia is that you will live, but you will [have] a poor quality [of] life,” Wazni says. “We can now improve that quality of life. We have learned that the basis of fibromyalgia and chronic fatigue has a lot to do with one’s hormonal and nutritional status, in addition to the underlying infection and [a] weak immune system.” Wazni adds that whether from illness or aging, there is a breakdown on the cellular level whereby cells do not receive the proper nutrition.
Dr. Edward Lichten, a Birmingham obstetrician/gynecologist, has spent years studying patterns in medicine, which he writes about in his book Textbook of Bio-Identical Hormones. He and Wazni see eye to eye. “Because all of their energy systems are off,” Lichten says, “these patients do not absorb the minerals, proteins, and fats you need to repair, restore, and have an active life. There’s a cycle causing more inflammation and more cellular degeneration.”
Lichten has found that six glands in the body — pineal, pituitary, thyroid, adrenal, pancreas, and gonads — regulate most bodily functions. “To treat disease,” he says, “you have to treat all six.”
Lichten has determined that fibromyalgia is caused by biological sleep disturbances due to low levels of vitamin D (which can cause insomnia), as well as by low levels of growth hormones in the pituitary gland. To treat fibromyalgia, patients are often given a concentrated form of vitamin D.
“We can prove it raises their blood levels,” Lichten says. “If you don’t sleep for a night, you wake up feeling stiff. If you don’t sleep well for a month, you feel like you ran a marathon all night.”
In addition, Lichten has found that most fibromyalgia patients have low thyroid levels, even after being put on thyroid medication. The result is that patients have little or no metabolism, making it difficult to heal bruised or overworked muscles. Often, the adrenal glands are overly taxed, which leaves patients feeling wired, as if they were perpetually over-caffeinated.
“These patients are physically and biologically exhausted,” Lichten says. “We proved this through blood tests. We give them DHEA (growth hormones), cortisol, and vitamin D, and it puts [the body] back in balance.” Each of the synthetic hormones (called bio-identical hormones) are custom-designed for each patient.”
Helen, a patient of Lichten’s who asked that her last name not be used because she fears retribution at her office, began getting fibromyalgia-type symptoms as a teenager, such as carpal-tunnel syndrome and allergies. But by her late 20s, she had pain in her hips, neck, lower back, and up and down her spine. As a professional, “I thought fibromyalgia was hooey,” she says, “something people used as an excuse to get out of work.” But as she sought medical treatment, she was continually dismissed, even as her insomnia grew to the point where she was barely getting four hours of sleep at night.
She covered it up at work, but came home each night, collapsing and crying. Concurrently, she was battling sinus infections and bronchitis that never seemed to clear up, despite repeated doses of antibiotics. She eventually learned it was because of a virus. “It’s a sign that your body is shutting down,” she says. “You feel like someone is [sending] a low-level electrical shock intermittently throughout your body. Now, every day, I take a nap and restore myself. When I nap, the infections go away. If I don’t, I don’t sleep at night.”
With the virus under control, Helen’s doctor began rebuilding and repairing her muscles by addressing her micronutrient deficiency through intravenous feeds. “If you have a body that doesn’t absorb nutrients, like I did, no matter what I ate, it wasn’t absorbing and I had no energy,” she says. “Now I feel like a new person.”
Men who are diagnosed with fibromyalgia have the same symptoms as women, but often receive different treatments. Not long ago, Dominick Mitchell, 49, an underwriter for Blue Cross Blue Shield, was a healthy, active, middle-aged man — a father and an avid weightlifter. But four years ago, he began suffering from aches and pains in his legs, which then traveled to his arms. Soon after, he noticed a strange lump under his ear, which he thought was a bug bite. Three weeks after noticing the lump, he developed strange, painful sensations in his arms and legs. Doctors tested him for multiple sclerosis, ALS, brain tumors, and more. Everything was negative, “but I still had the pain, and I got labeled as a nut,” he says. “I was able to work, because I was determined to, but it wasn’t fun. It really wears on your mind.”
A psychologist put him on low doses of antidepressants and muscle relaxants, but they, too, had no effect on the pain. His wife, obviously concerned, took him to her internist, Dr. Kathleen Norton, who practices at Beaumont Hospital in Royal Oak. The doctor thought he might have fibromyalgia, and referred him to Dr. Martin Pevzner of Oakland Arthritis Center in Bingham Farms, who confirmed the diagnosis. Pevzner put him on a painkiller for the pain cycles. Mitchell also called on Fibromyalgia & Fatigue Centers, where Wazni discovered that Mitchell’s hormones weren’t functioning correctly. Plus he had low testosterone levels and iron stores, which is common in middle-aged men. Through a combination of testosterone cream and injections of B-12, vitamin D, malic acid, omega-3, and other treatments, Mitchell is nearly healthy again. “I’m almost back to where I was before the fibromyalgia,” he says. “And if you exercise, you feel even better.”
Meloche, the therapist, has found that exercise has been a crucial part of her disease management, as well. “When I was a project manager, it would take every ounce of energy to get through the day,” she recalls. “You’re struggling, yet you look fine to everyone, so coworkers just think you’re a baby. Emotionally, that’s very tough. Sometimes you get foggy. You can look alert one day, and the next day, you’re out of it and you need more days off. People don’t always understand.”
Today, through regular exercise, massage therapy, and a better diet, among other things, Meloche has found a way to manage her fibromyalgia. She tries to do some form of exercise almost daily. “It’s very critical to do strength training, walking, and stretching,” she says. “I do yoga, because yoga does deeper stretching. Keeping my hip area and hamstrings stretched is the most important for me. It keeps my body balanced.”
Are You Suffering From Fibromyalgia?
Yes No Muscles stiff and painful
Yes No Experiencing numbness/tingling/stiffness
Yes No Recurring headaches
Yes No Can’t sleep
Yes No Tired and exhausted
Yes No Experiencing depression/sadness/anxiety
Yes No Unable to concentrate like you used to
Yes No Allergies/chemical sensitivities
Yes No Hormonal imbalance/PMS/menstrual pain
Yes No Sore throat/swollen glands
Yes No Stressed mentally/physically
Yes No Irritable-bowel or restless-leg syndrome
Yes No Experienced a traumatic event
Yes No History of infections
If you answered yes to:
1 to 3 questions: You’re experiencing a few of the common symptoms associated with fibromyalgia. Further testing is needed by a physician to determine if other conditions are a larger factor.
3 to 5 questions: You’re experiencing several of the symptoms commonly associated with fibromyalgia, as well as other potential conditions. Further testing is needed by a physician who specializes in diagnosing and treating these conditions to determine the most appropriate treatment.
5 or more questions: You’re experiencing a high number of the symptoms associated with fibromyalgia and should consider further evaluation by a physician who specializes in treating this condition.
Source: Fibromyalgia & Fatigue Center of Detroit; www.fibroandfatigue.com











